when a patient's respirations are shallow
 Respiratory rate 4: breathing rhythm and chest movement | Nursing Times
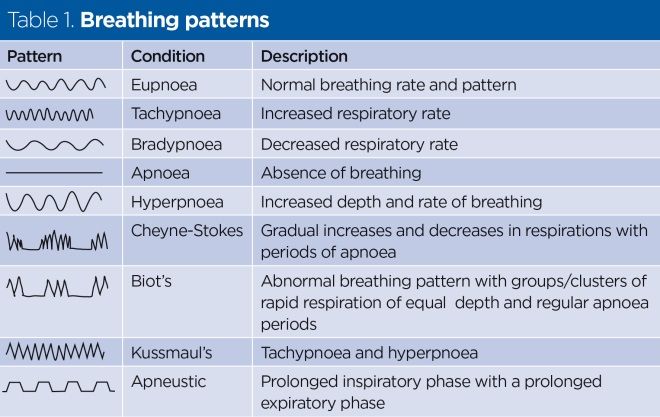
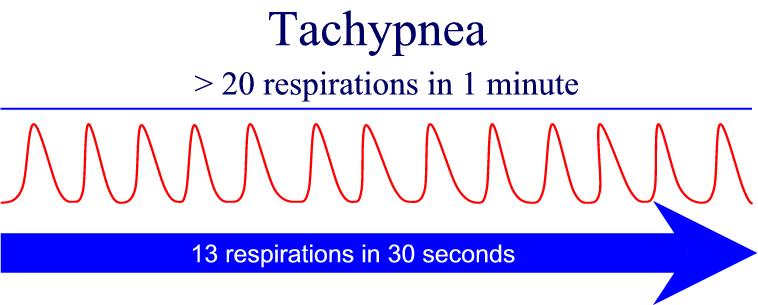
Respiratory rate 4: breathing rhythm and chest movement | Nursing TimesWarning: The NCBI website requires JavaScript to operate. NCBI Bookshelf. Service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan... StatPearls [Internet]. Abnormal Breaths Lacey Whited; Derrel D. Graham.AuthorsAfiliations Last updated: April 29, 2020. Continuous educational activity There are multiple types of normal and abnormal breathing. They include apnea, eupnea, orthopane, dyspnea, hyperpnea, hyperventilation, hypoventilation, tachypnea, breathing Kussmaul, breathing Cheyne-Stokes, breathing sigh, biot breathing, apneustic breathing, central neurogenic hyperventilation and central neurogenic hypoventilation. Each pattern is clinically important and useful for evaluating patients. This activity covers the essential characteristics of abnormal breathing and highlights the role of the interprofessional team in the care of patients affected by these conditions. Objectives:Introduction There are multiple types of normal and abnormal breathing. They include apnea, eupnea, orthopane, dyspnea, hyperpnea, hyperventilation, hypoventilation, tachypnea, breathing Kussmaul, breathing Cheyne-Stokes, breathing sigh, biot breathing, apneustic breathing, central neurogenic hyperventilation and central neurogenic hypoventilation. Each pattern is clinically important and useful for evaluating patients. FunctionAssessing respiratory patterns helps the clinician understand the current physiological condition of the patient. Abnormal respiratory patterns suggest the possibility of an underlying injury or metabolic misadjustments. Early examination of abnormal respiratory patterns can help the doctor intervene early to prevent further deterioration of the patient's condition. Concern ProblemsThe tissue is centrally controlled in the brain. It receives the entry of the central and peripheral chemoreceptors, as well as the voluntary control of the brain. The brain trunk also receives input from the chemoreceptors and adjusts the rate and tide volume based on pH and PaCO2. The regular cycle of breathing originates in medulla. The medular respiratory center has several widely dispersed groups of neurons that refer to the dorsal and ventral respiratory groups. There don't seem to be separate inspiring and expired centers. Bilateral dorsal respiratory groups control the rhythm of breathing by producing inspiring impulses. The neurons of this center send impulses to the neuron motors of the diaphragm and the external intercostal muscles. These nerves also extend to ventral respiratory groups (VRG). The entrance of the airways, lungs, joint thrusters and peripheral kimoreceptors through the vague and glyosophalyngeal nerves modifies the respiratory pattern. Ventral respiratory groups (VRG) are also bilateral collections of inspiring neurons and victors in medulla and are active in exercise and stress. These neurons send impulses to the external diaphragm and intercostals. They also stimulate the internal abdominal and intercostal muscles through neurons in the flow area. The interaction between the DRG and the VRG produces an impulse, the signal of the inspiring ramp. Starts low and gradual, then increases to produce a gentle inspiring effort. The pons contains two respiratory areas known as pneumotoxic and apneustic centers. The pneumotoxic center has an inhibiting effect on medulla. In fact, its stimulation causes the end of the inspiring effort and therefore controls the inspiring time. The weak signals of the pneumotoxic center increase the inspiring time causing an increase in the tide volume. The apneustic center stimulates the medulla-inspiring neurons and inhibits the victorious neurons. Overstimulation of this area produces long gaseous inspirations that are improperly interrupted by occasional expiration. This pattern is called apneustic breathing. Clinical Meaning The types of normal and abnormal clinically relevant breathing patterns include the following: Breath patterns associated with brain injury cannot be observed due to mechanical ventilation and sedation. There is a complex interaction in cases that result in brain injury. Self-regulation of the brain flow is affected by CO2 levels in the blood. As CO2 increases, the brain vessels are dilated, and as they decrease, the brain vessels will be limited. In traumatic brain injury (BIT), the brain is swollen and cannot be expanded due to the fixed volume of the skull intact. Increased intracranial pressure can overcome perfusion pressure by causing anoxia and injuries that lead to brain death and/or hernia. Although hyperventilation may lower PaCO2, causing vasoconstriction and reducing inflammation/CPI, it should be avoided. The effect is short-lived. In BIT, hyperventilation and hypoventilation should be avoided. The PCI is treated pharmacologically, surgically and with a medically induced coma. Improvement of Health Team Results All health workers must have some idea of what abnormal breathing is. There are several types of abnormal breathing and each has many causes. The key is to ensure that the appropriate specialist is promptly notified. Failure to recognize abnormal breathing can be fatal and lead to litigation. Continuous Education / Review QuestionsReferences This book is distributed under the terms of the Creative Commons 4.0 International License, which allows the use, duplication, adaptation, distribution and reproduction in any medium or format, provided that you give appropriate credit to the original author(s) and source, a link to the Creative Commons license is provided, and the changes made are indicated. ViewsIn this PageRelated information Similar products in PubMed Recent activityYour navigation activity is empty. The activity recording is off. , 8600 Rockville Pike, Bethesda MD, 20894 USA

Respiratory rate 4: breathing rhythm and chest movement | Nursing Times
4.4 What factors are noted when taking a patient's breathing rate and quality? | Taking Vital Signs
:max_bytes(150000):strip_icc()/what-is-a-normal-respiratory-rate-2248932-v1-5c1abe6846e0fb0001c6284a.png)
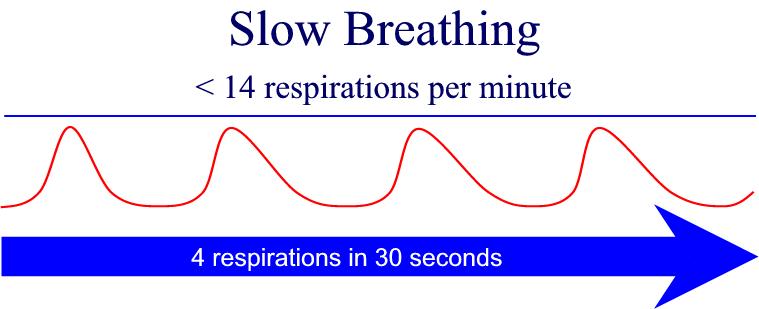
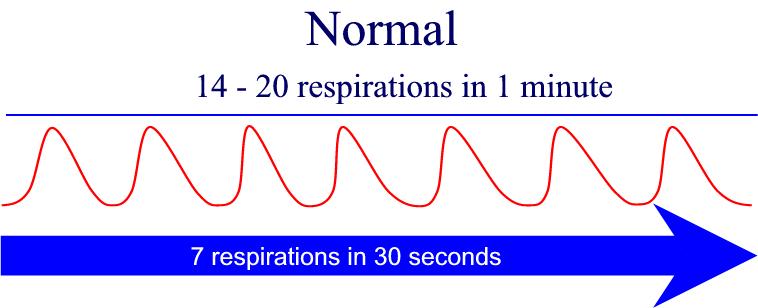
Normal Respiratory Rates in Adults and Children
4.4 What factors are noted when taking a patient's breathing rate and quality? | Taking Vital Signs
4.4 What factors are noted when taking a patient's breathing rate and quality? | Taking Vital Signs
Breathing Patterns in Respiratory Care (Abnormal and Irregular Patterns)

Respiratory rate 4: breathing rhythm and chest movement | Nursing Times

Kussmaul breathing - Wikipedia

Kussmaul breathing - Wikipedia
Physical Examination and Secondary Assessment (Principles of Clinical Practice) (Paramedic Care) Part 2

Ventilation vs Oxygenation vs Respiration: What is the Difference?

Shallow breathing - Wikipedia

Abnormal Breathing Patterns

Current clinical methods of measurement of respiratory rate give imprecise values | European Respiratory Society

Rapid Shallow Breathing: Causes, Treatments, and Prevention
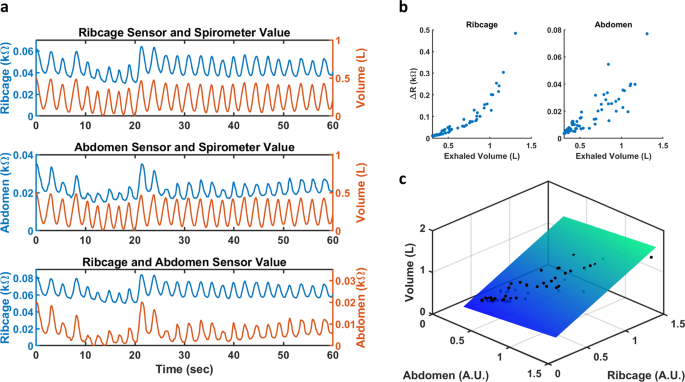
Respiration rate and volume measurements using wearable strain sensors | npj Digital Medicine

Respiratory rate 4: breathing rhythm and chest movement | Nursing Times
Kussmaul breathing - Wikipedia

Patient Assessment INITIAL ASSESSMENT. Patient Assessment 2 Components of the Initial Assessment Develop a general impression Assess mental status Assess. - ppt download

Post operative complications – Nursing 101
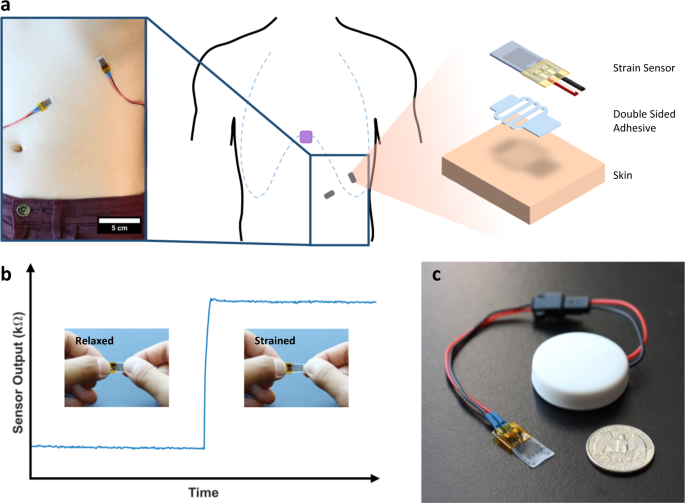
Respiration rate and volume measurements using wearable strain sensors | npj Digital Medicine

The importance of respiratory rate monitoring | British Journal of Nursing
Chapter 12 Illness in the elderly
Module 10: Vital Signs

How to Check Someone's Breathing Rate (Rate of Respiration)
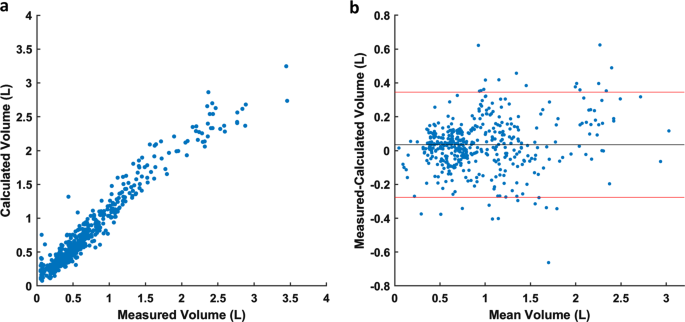
Respiration rate and volume measurements using wearable strain sensors | npj Digital Medicine

Guide to Vital Signs & Medical Assisting | Daymar College Blog

PDF) Association between the rapid shallow breathing index and extubation success in patients with traumatic brain injury

Mosby's Nursing Video Skills

How to Check Someone's Breathing Rate (Rate of Respiration)

Transthoracic Impedance Measurements in Patient Monitoring | Analog Devices
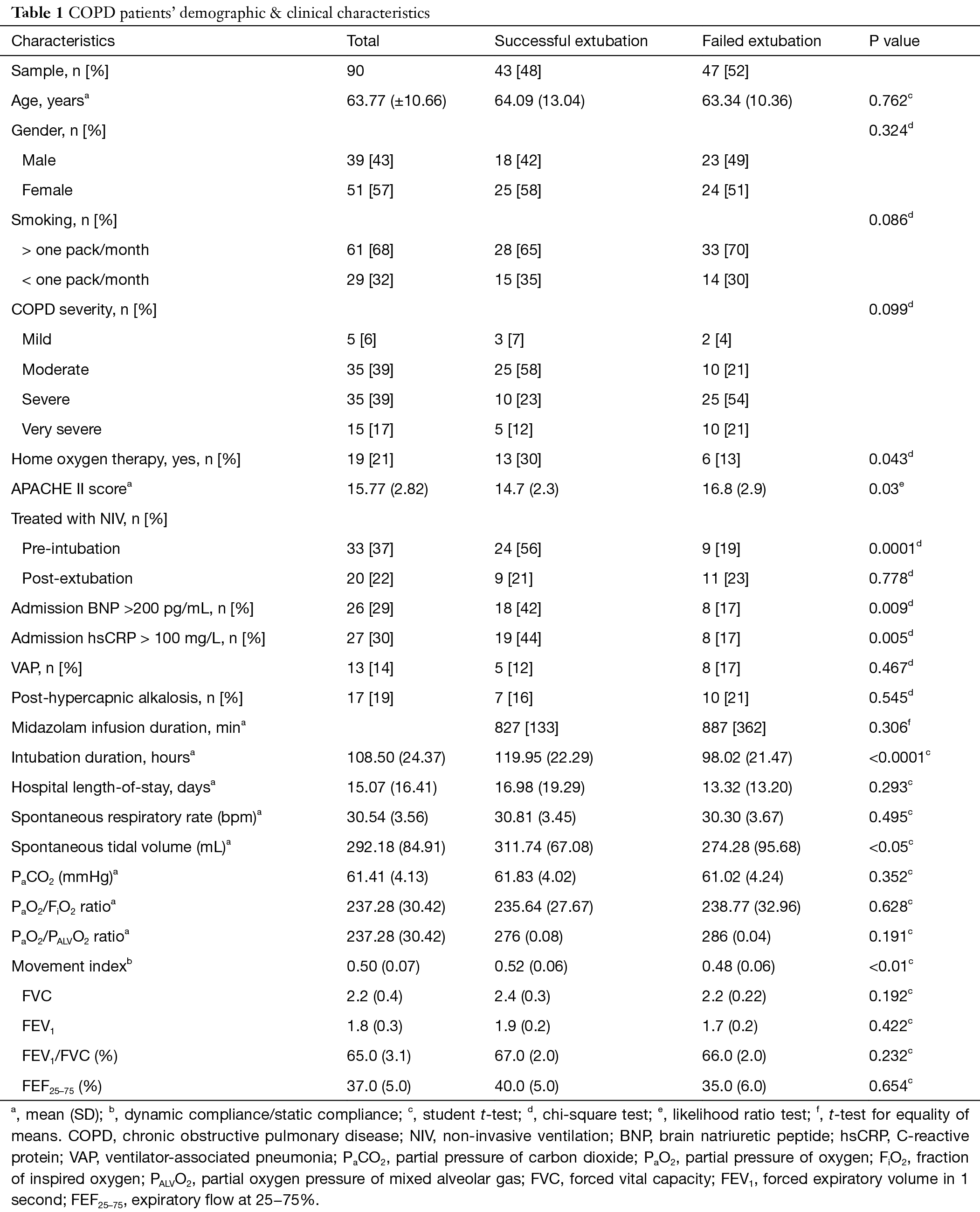
A rapid shallow breathing index threshold of 85 best predicts extubation success in chronic obstructive pulmonary disease patients with hypercapnic respiratory failure - Goharani - Journal of Thoracic Disease

PDF) Assessment of Rapid Shallow Breathing Index as a Predictor for Weaning in Respiratory Care Unit

Respiratory Rate - an overview | ScienceDirect Topics
Position-Dependent Pleural Friction Rub

How should we monitor patients with acute respiratory failure treated with noninvasive ventilation? | European Respiratory Society

Technical evaluation of different respiratory monitoring systems used for 4D CT acquisition under free breathing - Heinz - 2015 - Journal of Applied Clinical Medical Physics - Wiley Online Library
PPT - VITAL SIGNS/RESPIRATIONS علایم حیاتی Measure a Patient's Respirations (081-86A-0010) PowerPoint Presentation - ID:6206240

The art of anaesthesia . and very shallow respiration. The first trouble is usually noticeable at once. In thiscase the wooden mouth gag may be introduced, the teethseparated, and tip of tongue
Posting Komentar untuk "when a patient's respirations are shallow"